How to combat anaemia
Exhaustion, pale skin, shortness of breath … could it be anaemia? Read on for how to remedy this blood count abnormality which is much more common than you might think.

Anaemia: definition and symptoms
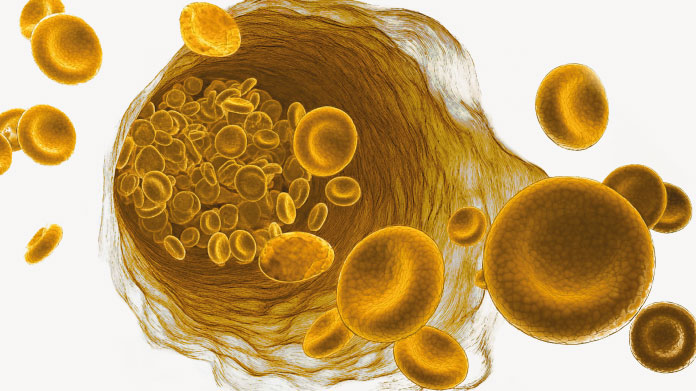
Anaemia describes an abnormal decrease in red blood cells (erythrocytes) or their depletion in haemoglobin (the protein responsible for transporting oxygen to the body’s organs) (1).
Mild anaemia often goes unnoticed, but as it worsens, it causes a number of symptoms related to poor oxygenation of tissues: shortness of breath on exertion, pale skin, intense fatigue, increased heart rate, dizziness, trouble concentrating... (2)
What causes anaemia?
In order to treat anaemia, it’s essential to first understand what’s causing it. Anaemia is either the result of defective red blood cell production in bone marrow (central causes), or loss or destruction of red blood cells by the body (peripheral causes).
Deficiency in iron remains the primary cause of diagnosed anaemia, affecting up to 1.5 billion people worldwide: this is unsurprisingly referred to as iron-deficiency anaemia(3). As a component of haem, this key mineral plays a direct role in the normal formation of red blood cells and haemoglobin. Pregnant women are more likely to be affected by this type of anaemia, as the growing foetus and greater blood volume results in increased iron requirements (4).
Anaemia may also be caused by a lack of either vitamin B9 or B12 (5-6), (both of which are necessary for red blood cell maturation), intestinal malabsorption of these vitamins (pernicious anaemia) (7), chronic inflammatory disease, kidney disease causing a deficiency in erythropoietin (EPO), or failure of bone marrow to produce blood cells (8).
Blood loss due to heavy periods or gastrointestinal bleeding are the most common peripheral causes of anaemia (9-10). In rarer cases, abnormalities in haemoglobin structure (seen in sickle-cell disease or thalassaemia) or antibody production directed against red blood cells cause premature destruction of erythrocytes, potentially inducing haemolytic anaemia (11).
What can you do to rapidly increase your iron levels?
Once a medical diagnosis of iron-deficiency anaemia has been confirmed, oral supplementation with iron is usually prescribed as a first-line treatment (12). Supplements should be taken in-between meals for at least 3 months.
When oral supplementation fails to correct the problem, in cases where loss of iron exceeds the body’s ability to absorb supplemental iron, or there is an underlying intestinal disorder, an intravenous iron infusion may be necessary (13).
How do you treat severe anaemia?
Sudden onset anaemia (following significant blood loss or surgery, for example) sometimes requires a blood transfusion (14). However, this carries a risk of complications and is therefore a treatment of last resort.
EPO injections are sometimes used in serious and chronic situations (dialysis, chemotherapy …) to stimulate bone marrow and treat anaemia while reducing the risks of transfusion (15).
How long does it take to successfully treat anaemia?
A person being treated for iron-deficiency anaemia should see an improvement in their symptoms within a few weeks.
To assess the treatment’s efficacy, blood tests are taken to check the patient’s haemoglobin levels which usually return to normal within 6-8 weeks. Their levels of ferritin (a marker of the body’s iron reserves) will also be checked three months after the start of treatment: normal levels usually mean supplementation can cease (16).
What should you eat if you’re anaemic?
If you’re anaemic, it’s obviously important to adopt a diet that contains sufficient iron, but also one that provides plenty of vitamin B9 (green leafy vegetables, pulses…) and vitamin B12 (animal-source foods).
Offal and red meat
With 16.1mg/100g, black pudding is justifiably top of the list of iron-rich foods. Calves’ liver and red meat are also good sources, which can be consumed twice a week (17).
In terms of plant-origin foods, soya beans and tofu (2.4mg/100g) are respectable sources, though they’re a long way off nori seaweed with 234mg/100g (18). Be aware that non-haem iron (from plant-source foods, eggs and milk) is less well-absorbed by the body than haem iron (from meat products).
Iron-rich fruits
Fresh fruit naturally contains little iron. Oil seeds and oleaginous fruits (such as sesame seeds, almonds, hazelnuts…) and dried fruits (such as dried figs) fare a little better. Conversely, citrus fruits, peppers and kiwi fruit, with their high levels of vitamin C, help to boost absorption of iron from plant-source foods when consumed as part of a meal (19).
Iron-rich vegetables
Spinach is a fairly good source, offering 3.61mg/100g, though pulses (lentils, flageolet beans, red kidney beans…) contain almost twice as much. Topping the list, however, are dried aromatic herbs such as thyme (124mg/100g) (20).
Ginger, and even more so, cumin, fenugreek and turmeric, have a particularly high iron content (21). Even when consumed in small quantities, these spices conveniently combine with the iron provided by other foods over a day. Other good dietary sources are cocoa powder and dark chocolate.
Anaemia: foods to avoid
It’s now recognised that the tannins in tea (as well as in grapes and red berries) inhibit good iron absorption, as do the phytates in grains and legumes(22-23). So if you’re anaemic, it’s wise to leave a gap between consuming these foods and taking your iron supplements.
Treating anaemia: which supplements should you choose?
Iron supplementation should only be started once anaemia has been confirmed by a blood test, since excess iron levels are harmful to health. Once there is a clear diagnosis of iron deficiency, it’s then a good idea to take a safe and effective iron supplement.
Some forms of iron, such as ferrous sulphate, ferric citrate or iron D-gluconate, are associated with a number of adverse side-effects including stomach problems(24). Iron bisglycinate (found in the supplement Iron Bisglycinate) is not only very well tolerated but also offers optimal bioavailability because it has a low molecular weight and no ion charge (which reduces interactions with other nutrients) (25).
When anaemia is due to a lack of folates (malnutrition, pregnancy, cytotoxic drugs …) or vitamin B12 (strict vegan diet), targeted supplementation can be initiated, but always with your doctor’s approval (try, for example, SuperFolate 200 mcg for vitamin B9 or Methylcobalamine for vitamin B12).
SUPERSMART ADVICE
References
- Turner J, Parsi M, Badireddy M. Anemia. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499994/
- Chaparro CM, Suchdev PS. Anemia epidemiology, pathophysiology, and etiology in low- and middle-income countries. Ann N Y Acad Sci. 2019 Aug;1450(1):15-31. doi: 10.1111/nyas.14092. Epub 2019 Apr 22. PMID: 31008520; PMCID: PMC6697587.
- Warner MJ, Kamran MT. Iron Deficiency Anemia. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448065/
- Georgieff MK. Iron deficiency in pregnancy. Am J Obstet Gynecol. 2020 Oct;223(4):516-524. doi: 10.1016/j.ajog.2020.03.006. Epub 2020 Mar 14. PMID: 32184147; PMCID: PMC7492370.
- Ankar A, Kumar A. Vitamin B12 Deficiency. [Updated 2022 Oct 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441923/
- Merrell BJ, McMurry JP. Folic Acid. [Updated 2022 Dec 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK554487/
- Vaqar S, Shackelford K. Pernicious Anemia. [Updated 2023 Mar 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK540989/
- Moore CA, Krishnan K. Bone Marrow Failure. [Updated 2022 Jul 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459249/
- Kocaoz S, Cirpan R, Degirmencioglu AZ. The prevalence and impacts heavy menstrual bleeding on anemia, fatigue and quality of life in women of reproductive age. Pak J Med Sci. 2019 Mar-Apr;35(2):365-370. doi: 10.12669/pjms.35.2.644. PMID: 31086516; PMCID: PMC6500811.
- Cotter J, Baldaia C, Ferreira M, Macedo G, Pedroto I. Diagnosis and treatment of iron-deficiency anemia in gastrointestinal bleeding: A systematic review. World J Gastroenterol. 2020 Dec 7;26(45):7242-7257. doi: 10.3748/wjg.v26.i45.7242. PMID: 33362380; PMCID: PMC7723662.
- Sedrak A, Kondamudi NP. Sickle Cell Disease. [Updated 2022 Aug 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482384/
- Nguyen M, Tadi P. Iron Supplementation. [Updated 2022 Jul 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557376/
- Lima J, Gago P, Rocha M, Grilo I, Gomes R, Luís M, Sarmento T, Teira A, Sousa M, Barbosa M. Role of intravenous iron in the treatment of anemia in patients with gastrointestinal tract tumors undergoing chemotherapy: a single-center, observational study. Int J Gen Med. 2018 Aug 22;11:331-336. doi: 10.2147/IJGM.S165947. PMID: 30197530; PMCID: PMC6112805.
- Lotterman S, Sharma S. Blood Transfusion. [Updated 2022 Jun 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499824/
- Schoener B, Borger J. Erythropoietin Stimulating Agents. [Updated 2023 Mar 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK536997/
- Knovich MA, Storey JA, Coffman LG, Torti SV, Torti FM. Ferritin for the clinician. Blood Rev. 2009 May;23(3):95-104. doi: 10.1016/j.blre.2008.08.001. Epub 2008 Oct 2. PMID: 18835072; PMCID: PMC2717717.
- org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-. How can I get enough iron? 2014 Mar 20 [Updated 2018 Mar 22]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279618/
- Bhatnagar RS, Miller DD, Padilla-Zakour OI, Lei XG. Supplemental Microalgal Iron Helps Replete Blood Hemoglobin in Moderately Anemic Mice Fed a Rice-Based Diet. 2020 Jul 27;12(8):2239. doi: 10.3390/nu12082239. PMID: 32727043; PMCID: PMC7468699.
- Lynch SR, Cook JD. Interaction of vitamin C and iron. Ann N Y Acad Sci. 1980;355:32-44. doi: 10.1111/j.1749-6632.1980.tb21325.x. PMID: 6940487.
- Hammoudi Halat D, Krayem M, Khaled S, Younes S. A Focused Insight into Thyme: Biological, Chemical, and Therapeutic Properties of an Indigenous Mediterranean Herb. 2022 May 18;14(10):2104. doi: 10.3390/nu14102104. PMID: 35631245; PMCID: PMC9147557.
- Ooi SL, Pak SC, Campbell R, Manoharan A. Polyphenol-Rich Ginger (Zingiber officinale) for Iron Deficiency Anaemia and Other Clinical Entities Associated with Altered Iron Metabolism. 2022 Sep 28;27(19):6417. doi: 10.3390/molecules27196417. PMID: 36234956; PMCID: PMC9573525.
- Disler PB, Lynch SR, Charlton RW, Torrance JD, Bothwell TH, Walker RB, Mayet F. The effect of tea on iron absorption. 1975 Mar;16(3):193-200. doi: 10.1136/gut.16.3.193. PMID: 1168162; PMCID: PMC1410962.
- Piskin E, Cianciosi D, Gulec S, Tomas M, Capanoglu E. Iron Absorption: Factors, Limitations, and Improvement Methods. ACS Omega. 2022 Jun 10;7(24):20441-20456. doi: 10.1021/acsomega.2c01833. PMID: 35755397; PMCID: PMC9219084.
- Tolkien Z, Stecher L, Mander AP, Pereira DI, Powell JJ. Ferrous sulfate supplementation causes significant gastrointestinal side-effects in adults: a systematic review and meta-analysis. PLoS One. 2015 Feb 20;10(2):e0117383. doi: 10.1371/journal.pone.0117383. PMID: 25700159; PMCID: PMC4336293.
- Name JJ, Vasconcelos AR, Valzachi Rocha Maluf MC. Iron Bisglycinate Chelate and Polymaltose Iron for the Treatment of Iron Deficiency Anemia: A Pilot Randomized Trial. Curr Pediatr Rev. 2018;14(4):261-268. doi: 10.2174/1573396314666181002170040. PMID: 30280670; PMCID: PMC6416187.
Keywords
62 Days
Very happy with the order and the…
Very happy with the order and the prompt team's response to an identified issue with my order.
KUQI Fatmir
69 Days
15 + years as a customer
I have been using their products for over 15 years as I find both the quality and pricing excellent.
Del Chandler
71 Days
Good quick delivery
Good quick delivery
Timothy O Shea
72 Days
Good service
Good communication following order. Product came within the time frame and was well packaged. The only confusing thing I found was in checking out. For some reason it is not clear how to do so and the current system should be improved.
Joe O Leary
81 Days
Simple and fast.
Simple and fast.
Nina
82 Days
Great product was definitely what is…
Great product was definitely what is says and arrived on without issue
customer
88 Days
I love reading those product facts on…
I love reading those product facts on Supersmart.com. Effective health products making permanent changes to my blood-work results and testes. However, I also have to order capsules from other websites.
NORDGULEN Olav
90 Days
Great products
Great products Very easy to choose, to order… and to get at home
Federica mastrojanni
93 Days
Service rapide et bons produits
Service rapide et bons produits
customer
94 Days
Good products and fast delivery
Good products and fast delivery
Trusted
99 Days
Does what it says on the can
I believe in this product Made to highest standard The ordering process is straightforward Delivery time prompt Excellent product, excellent service Happy customer ❤️
Sheba Kelleher
104 Days
Excellents produits
Excellents produits. Rien à dire si ce n'est qu'ils sont très chèrs.
MJS_France
106 Days
Very good supplement
Very good supplement
Glaveash
107 Days
Supersmart supplements are really…effective
Supersmart supplements are really effective and have helped me and family members and friends to improve their health including some of us with severe health problems including some with no existing medical treatment.
Anne Georget
109 Days
SuperBig Supersmart
SuperBig Supersmart
Pierre