Excess iron in the blood: is it serious?
Iron is a mineral which the body needs in order to function properly. It supports the production of red blood cells which transport oxygen to all the body’s tissues.
Iron absorption in the gut is normally in line with the body’s needs and no more. So an overly iron-rich diet will not theoretically lead to excess iron in the blood as only the amount needed by the body is absorbed.
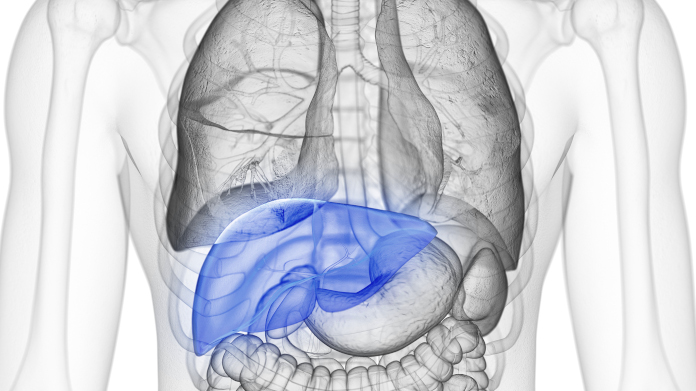
Sometimes, however, this absorption mechanism is defective and the body absorbs more iron than necessary. The surplus is then stored in the liver, pancreas and heart. Over the long term, this can result in an abnormal build-up of iron in organs, producing side effects, symptoms and serious damage:
- cirrhosis, then cancer of the liver;
- disease of the heart muscle (cardiomyopathy), then heart failure;
- abnormal insulin production, then diabetes.
Excess iron can also produce other symptoms: erectile dysfunction (iron deposits in the testicles), joint disorders, fatigue, abnormal skin pigmentation (‘bronze diabetes’), bone damage, hair loss … These can appear gradually with organ damage.
What are the possible causes of excess iron in the blood?
As mentioned, an iron-heavy diet will not normally lead to excess iron in the blood, even over the long term. Elevated iron in the blood is always a sign of another health problem or a repeated practice.
The most common causes of iron overload are:
- haemochromatosis, a genetic condition causing excessive iron absorption. It affects 1 in 200-300 people in Europe, mainly men. Symptoms usually appear after the age of 40, though children can sometimes be affected. Diagnosis can be confirmed with a genetic test (mutation C282Y);
- excessive alcohol consumption which increases the absorption of iron and damages the liver, reducing its ability to regulate iron levels in the body;
- liver disease which interferes with iron metabolism;
- long-term use of dietary supplements containing high levels of iron;
- repeated blood transfusions (transfusional hemosiderosis). Each bag (or ‘unit of blood’) contains about 250mg of iron;
- other rare diseases such as haemoglobinopathies (difficulty producing red blood cells) and myelodysplasia (bone marrow disease), etc.
What should you do if you suspect you have iron overload?
Blood test and ferritin assay
If you think you may have too much iron in your blood, you should contact your GP.
A serum ferritin level test (following a blood test) will usually be carried out as a first step. Ferritin is the protein responsible for storing iron in the body (up to 4500 iron atoms per protein): abnormally high levels in the blood may suggest elevated iron stores in the body (1).
However, as ferritin is also an inflammatory marker, it’s important to note that a high level does not necessary reflect iron overload. It can also be the result of chronic alcoholism, chronic inflammation, a traumatic event causig cell destruction, and metabolic syndrome (excess visceral fat in the abdominal region).
Transferrin saturation level test
In the case of elevated ferritin, it’s therefore important to check the transferrin saturation level too, transferrin being the protein responsible for transporting iron across the intestinal wall. Transferrin saturation is normally less than 45%, but can go above 75% when iron absorption is abnormally high.
Depending on the results, your healthcare professional can then refer you for further tests such as a liver MRI to assess the extent of your organ overload.
In the case of diagnosed iron overload, what happens next?
Treatment of iron overload depends on the diagnosis: under no circumstances should you self-medicate to reduce your iron stores.
Your health professional may recommend intravenous medication (such as deferoxamine) which binds to iron to eliminate it from the body in urine. This is called iron chelation.
Depending on the cause, he or she may equally employ a procedure in which small amounts of blood are repeatedly drawn from a vein to gradually remove the excess iron: this is known as phlebotomy or venesection.
At the same time, it’s obviously important to treat the cause of the excess iron storage.
Are there natural ways of reducing excess iron? What should you eat?
Most of the time, there is no need to reduce your consumption of iron-containing foods such as red meat, as excess iron is a problem of absorption rather than intake (2-3).
However, there are some nutritional tips you may want to adopt:
- obviously avoid iron supplements, but also steer clear of foods enriched with iron such as processed breakfast cereals;
- avoid supplements containing vitamin C too, and therefore multivitamins, as they increase iron absorption in the gut. In the same vein, avoid vitamin C-rich foods and drinks (like citrus fruit juices) at mealtimes;
- consider consuming foods or drinks which can reduce iron absorption such as green tea, coffee (but not in excess), turmeric (which is also a potential iron chelator, ie, able to bind to iron to facilitate its excretion), those rich in both calcium such as milk and tofu, and zinc such as pumpkin seeds, cashew nuts and yogurt (though zinc supplements should be avoided if you have haemochromatosis as the condition increases zinc absorption excessively). and those rich in dietary fibre like wheat bran. All of these should ideally be consumed with a meal;
- taking a green tea supplement (such as EGCG) or one containing turmeric (Super Curcuma) is also an option but only under medical supervision;
- limit your consumption of alcohol to reduce both your iron absorption and the deterioration of your already iron-saturated liver;
- limit your consumption of iron-rich offal to no more than once a week.
The opposite case: iron deficiency
Finally, it’s worth noting that the opposite case, a lack of iron, is much more common than iron overload. In fact, hyperferritinaemia is often discovered by accident, during a test for iron deficiency.
When iron deficiency has been confirmed by a blood test, and depending on your doctor’s advice, you could supplement with iron bisglycinate, a highly-bioavailable form effective at increasing your iron intake (you’ll find it in the supplement Iron Bisglycinate).
SUPERSMART ADVICE
References
- Saglini, V., Brissot, P., Hyperferritinémie – Algorithme, Rev Med Suisse, 2012/342 (Vol.8), p. 1135–1137. DOI: 10.53738/REVMED.2012.8.342.1135 URL: https://www.revmed.ch/revue-medicale-suisse/2012/revue-medicale-suisse-342/hyperferritinemie-algorithme
- Bacon BR, Adams PC, Kowdley KV, Powell LW, Tavill AS; American Association for the Study of Liver Diseases. Diagnosis and management of hemochromatosis: 2011 practice guideline by the American Association for the Study of Liver Diseases. Hepatology. 2011 Jul;54(1):328-43. doi: 10.1002/hep.24330. PMID: 21452290; PMCID: PMC3149125.
- Barton JC, McDonnell SM, Adams PC, Brissot P, Powell LW, Edwards CQ, Cook JD, Kowdley KV. Management of hemochromatosis. Hemochromatosis Management Working Group. Ann Intern Med. 1998 Dec 1;129(11):932-9. doi: 10.7326/0003-4819-129-11_part_2-199812011-00003. PMID: 9867745.
55 Days
Very happy with the order and the…
Very happy with the order and the prompt team's response to an identified issue with my order.
KUQI Fatmir
62 Days
15 + years as a customer
I have been using their products for over 15 years as I find both the quality and pricing excellent.
Del Chandler
64 Days
Good quick delivery
Good quick delivery
Timothy O Shea
65 Days
Good service
Good communication following order. Product came within the time frame and was well packaged. The only confusing thing I found was in checking out. For some reason it is not clear how to do so and the current system should be improved.
Joe O Leary
74 Days
Simple and fast.
Simple and fast.
Nina
74 Days
Great product was definitely what is…
Great product was definitely what is says and arrived on without issue
customer
81 Days
I love reading those product facts on…
I love reading those product facts on Supersmart.com. Effective health products making permanent changes to my blood-work results and testes. However, I also have to order capsules from other websites.
NORDGULEN Olav
83 Days
Great products
Great products Very easy to choose, to order… and to get at home
Federica mastrojanni
86 Days
Service rapide et bons produits
Service rapide et bons produits
customer
87 Days
Good products and fast delivery
Good products and fast delivery
Trusted
92 Days
Does what it says on the can
I believe in this product Made to highest standard The ordering process is straightforward Delivery time prompt Excellent product, excellent service Happy customer ❤️
Sheba Kelleher
97 Days
Excellents produits
Excellents produits. Rien à dire si ce n'est qu'ils sont très chèrs.
MJS_France
99 Days
Very good supplement
Very good supplement
Glaveash
100 Days
Supersmart supplements are really…effective
Supersmart supplements are really effective and have helped me and family members and friends to improve their health including some of us with severe health problems including some with no existing medical treatment.
Anne Georget
101 Days
SuperBig Supersmart
SuperBig Supersmart
Pierre