What are the 4 worst foods for osteoarthritis?
Osteoarthritis, a real scourge for people over 45, remains incurable to this day. The best strategy is to alleviate the symptoms and slow down its progression, in particular, by avoiding food traps. Discover today the 4 foods to avoid as much as possible to stay in control of the situation.
Nutritional management of osteoarthritis
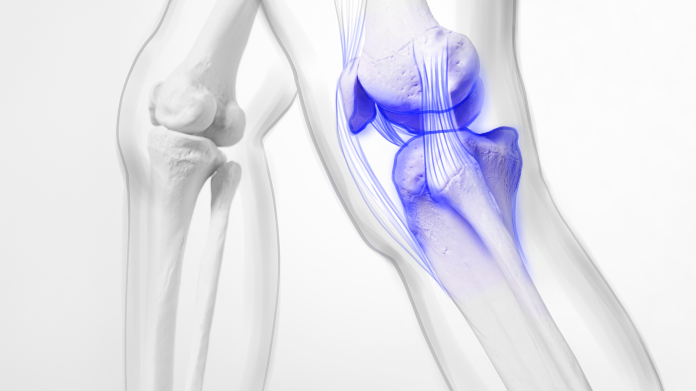
What is osteoarthritis?
Affecting more than 10% of the world's population and a quarter of people over the age of 45, osteoarthritis is a chronic degenerative disease marked by the progressive and irreversible destruction of cartilage in the joints.
It progresses in phases and through painful flare-ups, at an unpredictable rate.
It is the leading cause of locomotor disability in the over-65s, with the fingers, knees and hips being the areas most affected.
How can we prevent osteoarthritis or slow its progression through diet?
Diet plays a key role in preventing and managing osteoarthritis.
By adopting good eating habits, you can reduce inflammation and preserve your joints for longer.
Here are 5 essential recommendations:
- Increase your intake of foods rich in omega-3s, such as oily fish, seafood, avocado and nuts (especially walnuts). These essential fatty acids are thought to help fight inflammation (1).
- Increase your fibre intake. The addition of 5 to 10 grams of soluble fibre per day can reduce serum cholesterol, which plays a role in the development of osteoarthritis, by 5 to 10%.
- Eat a healthy, balanced diet to avoid excess weight and especially abdominal obesity: each kilogram of excess weight increases the risk of osteoarthritis by 10% (2). Regular, appropriate physical activity is also strongly recommended.
- Ensure that you have an optimal intake of vitamin D. This vitamin contributes to the absorption and normal use of calcium, helping to maintain good bone health. As a result, it can reduce stress and wear on cartilage. It can be found in oily fish and egg yolks, through exposure to the sun, etc. (3).
- Consume sources of collagen, the key compound in joint cartilage. Try bone broth, lean meats, various fish with skin (salmon, mackerel, tuna, etc.).
The 4 worst foods for promoting or aggravating osteoarthritis
Just as there are no miracle foods capable of providing instant relief from osteoarthritis attacks, there are no real 'trigger' foods with immediate and dramatic effects on the disease.
Nonetheless, we have tried to highlight the mechanisms by which the disease worsens and progresses through chronic phases.
Alcohol: public enemy number 1 for all diseases, including osteoarthritis
Alcohol consumption is a well-known risk factor for a number of major diseases, such as cardiovascular disease, cancer and... osteoarthritis.
Alcohol contributes to the worsening of osteoarthritis by 3 mechanisms:
- increasing systemic inflammation (due to excessively high triglycerides) (4);
- contributing to abdominal obesity, which produces pro-inflammatory adipokine, harmful to joints;
- disrupting cartilage repair, particularly by interfering with metabolic processes (5).
A large-scale meta-analysis showed that regular alcohol consumption significantly and indisputably increased the risk of suffering premature osteoarthritis (6).
Industrially fried foods and cold meats: boosters of osteoarthritis
Saturated fats and trans fats should be substantially reduced in cases of osteoarthritis, as they exacerbate inflammation and the associated pain.
But that's not all: studies show that an increase in total fat and saturated fatty acids is associated with increased joint loss, while an increase in monounsaturated fatty acids and polyunsaturated fatty acids ('good fats') is associated with improved function.
Put another way, sources of saturated fats such as cold meats (sausages, pâté, etc.) increase pain in the short term and aggravate osteoarthritis in the long term.
Industrially fried foods such as doughnuts and nuggets, often prepared in partially hydrogenated oils, are one of the most important sources of these bad fats.
Here are some other examples of sources of trans fatty acids and saturated fatty acids to limit:
- butter, cream and cheeses (especially soft cheeses);
- palm oil and coconut oil;
- red and fatty meats (beef, pork, lamb);
- industrial bakery products;
- hydrogenated margarines, etc.
Sugary drinks: dramatically pro-inflammatory
Simple sugars (glucose, fructose, sucrose, lactose, maltose, etc.) and products with a high glycaemic index have a pro-inflammatory effect on the body.
They exacerbate the symptoms of inflammation and, therefore, contribute to the acute pain of osteoarthritis.
Furthermore, excess carbohydrate intake is converted in the body into saturated fatty acids, which are then stored as triglycerides.
High triglyceride levels are catastrophic for osteoarthritis: they encourage the production of pro-inflammatory cytokines, increase oxidative stress (which damages joint cartilage), contribute to abdominal obesity (which increases the mechanical load on joints) and disrupt the production of hormones secreted by adipose tissue.
Sugary drinks (soft drinks, energy drinks, industrial fruit juices, etc.), while of little nutritional benefit, are among the foods that contain the most sugars: 30 to 40 g of sugars per 33 cL.
Here are some other foods rich in simple sugars to limit:
- confectionery (sweets, chocolate bars, etc.);
- cakes, biscuits and pastries (30-40g of sugar per 100g);
- syrups;
- sweetened cereals;
- ice cream and frozen desserts.
Coffee (and even decaffeinated coffee)
This is the surprise entry on the list: according to certain studies, coffee is also linked to an increased risk of osteoarthritis (7).
The caffeine it contains is suspected of damaging joint health by increasing the production of osteoclasts, which promote bone breakdown, thereby compromising joint stability and accelerating the wear and tear of cartilage.
What's more, caffeine can interfere with adenosine receptors, which play a role in reducing inflammation.
Even more surprising, however, is the fact that caffeine-free coffee is, according to some researchers, potentially associated with an even greater risk.
How can this paradox be explained? It's possible that the decaffeination process affects the beneficial compounds in coffee (such as polyphenols) while retaining certain molecules that can harm joints.
However, this conclusion may stem from a causal bias: consumers of decaffeinated coffee are often former heavy caffeinated coffee drinkers who have had to reduce their consumption.
Regardless, in cases of osteoarthritis, it is recommended to limit coffee consumption to 1 or 2 cups a day maximum. However, the link between coffee and osteoarthritis remains to be studied further.
Ideal food supplements for osteoarthritis
There are many natural substances of interest for joint health:
- omega-3 fatty acids. Already mentioned at the beginning of this article, they help to restore the correct balance between omega-3 and omega-6, and also help to maintain a normal concentration of triglycerides in the blood (discover the Super Omega 3 supplement, a pure and stable source of EPA and DHA);
- MSM. This compound provides you with organic sulphur, essential for the synthesis of chondroitin, glucosamine and hyaluronic acid, which naturally promote joint lubrication (ideally choose OptiMSM®, an extremely pure, vegetarian and GMO-free MSM supplement);
- collagen. Already mentioned above, collagen is a structural protein essential to the functioning of cartilage and joints. In the event of joint problems, focus in particular on type 2 collagen (for example with UC II®);
- vitamin C. This well-known vitamin contributes to the normal formation of collagen, thus helping cartilage to function normally (opt, for example, for the Ester C® supplement, whose vitamin C is designed to last longer);
- Boswellia serrata extract. Boswellia is a plant traditionally used for its anti-inflammatory properties, particularly for joint problems. It is available as a single-ingredient supplement (such as Super Boswellia) or as a formula (such as Flexi-Smart, which combines boswellia extract with hyaluronic acid and avocado and soya unsaponifiables);
- vitamin D. As mentioned above, vitamin D helps maintain normal bones and is therefore beneficial to joints (opt for Vitamin D3 5000 IU, a high-dose vitamin D3 supplement);
- tabashir bamboo extract. This silica-rich extract promotes joint health by strengthening cartilage and reducing inflammation.
Some joint formulas combine several of these compounds: vitamin C, bamboo extract, MSM, etc. (take advantage of Joint Support Formula, for example, which contains hyaluronic acid, chondroitin, glucosamine and manganese in addition to all these ingredients). It's a good idea to use more than one substance, as long as they work in synergy, to give yourself the best chance of success.
SUPERSMART ADVICE
References
- Jordi Salas-Salvado, Christopher Papandreou et al. The Mediterranean Diet - An evidence-base approach, second edition. Elsevier. Elsevier; 2020. 588 p.
- Huffman KF, Thornhill TH, Ambrose KR, Nelson AE, Callahan LF. Osteoarthritis and Its Management: What the Physician Assistant Needs to Know. Physician Assist Clin. 1 janv 2021;6(1):23‑40.
- Guillot X, Semerano L, Saidenberg-Kermanac’h N, Falgarone G, Boissier M-C. Vitamine D et inflammation. Rev Rhum. 1 mars 2011;78(2):128‑33
- Volcik KA, Ballantyne CM, Fuchs FD, Sharrett AR, Boerwinkle E. Relationship of alcohol consumption and type of alcoholic beverage consumed with plasma lipid levels: differences between Whites and African Americans of the ARIC study. Ann Epidemiol. 2008;18(2):101–7.
- Wen MT, Liang XZ, Luo D, Li JC, Yan BZ, Lu BW, Xu B, Li G. Plasma lipids, alcohol intake frequency and risk of Osteoarthritis: a Mendelian randomization study. BMC Public Health. 2023 Jul 11;23(1):1327. doi: 10.1186/s12889-023-16250-1. PMID: 37434151; PMCID: PMC10337179.
- To K, Mak C, Zhang C, Zhou Y, Filbay S, Khan W. The association between alcohol consumption and osteoarthritis: a meta-analysis and meta-regression of observational studies. Rheumatol Int. 2021;41(9):1577–91.
- Zhang W, Lei X, Tu Y, Ma T, Wen T, Yang T, Xue L, Ji J, Xue H. Coffee and the risk of osteoarthritis: a two-sample, two-step multivariable Mendelian randomization study. Front Genet. 2024 Feb 1;15:1340044. doi: 10.3389/fgene.2024.1340044. PMID: 38362204; PMCID: PMC10867243.
64 Days
Very happy with the order and the…
Very happy with the order and the prompt team's response to an identified issue with my order.
KUQI Fatmir
71 Days
15 + years as a customer
I have been using their products for over 15 years as I find both the quality and pricing excellent.
Del Chandler
73 Days
Good quick delivery
Good quick delivery
Timothy O Shea
74 Days
Good service
Good communication following order. Product came within the time frame and was well packaged. The only confusing thing I found was in checking out. For some reason it is not clear how to do so and the current system should be improved.
Joe O Leary
83 Days
Simple and fast.
Simple and fast.
Nina
84 Days
Great product was definitely what is…
Great product was definitely what is says and arrived on without issue
customer
90 Days
I love reading those product facts on…
I love reading those product facts on Supersmart.com. Effective health products making permanent changes to my blood-work results and testes. However, I also have to order capsules from other websites.
NORDGULEN Olav
92 Days
Great products
Great products Very easy to choose, to order… and to get at home
Federica mastrojanni
95 Days
Service rapide et bons produits
Service rapide et bons produits
customer
96 Days
Good products and fast delivery
Good products and fast delivery
Trusted
101 Days
Does what it says on the can
I believe in this product Made to highest standard The ordering process is straightforward Delivery time prompt Excellent product, excellent service Happy customer ❤️
Sheba Kelleher
106 Days
Excellents produits
Excellents produits. Rien à dire si ce n'est qu'ils sont très chèrs.
MJS_France
108 Days
Very good supplement
Very good supplement
Glaveash
109 Days
Supersmart supplements are really…effective
Supersmart supplements are really effective and have helped me and family members and friends to improve their health including some of us with severe health problems including some with no existing medical treatment.
Anne Georget
110 Days
SuperBig Supersmart
SuperBig Supersmart
Pierre